Assessment of care needs
Care need assessment is a systematic process of identifying and addressing the patient’s needs to the gaps in their present care and the required care for them. Grimsley and Allison (2016) state that accurately measuring the difference between the current care and desired care is crucial for identifying the care gaps and the factors that are inhibiting practical care. It is particularly vital for patients with mental health issues as their care needs change, which decreases their care quality.
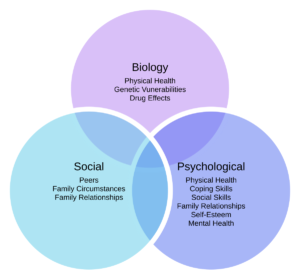
In the present scenario, the patient’s name will be pseudonymised following Corus’ Domains and Proficiencies for social workers, which include patients’ confidentiality as a core social worker’s ability. Mr Higgins was diagnosed with Korsakoff’s Syndrome; lately; the complete case study is added in appendix A below. To deliver accurate and needed care for him, a Community Mental Health Team was devised, and I was assigned the role of his social worker. Before offering him the needed care, the nurses conducted his comprehensive health need assessment. Campion, Coombes, and Bhaduri (2017) stated that in the United Kingdom (UK), less than half of patients with mental health issues can access healthcare services. It is due to poor need assessment where the practitioners cannot grasp the biopsychosocial needs of patients and deliver care for only a single aspect. Hence, the present essay will use a biopsychosocial approach for his care process. The biopsychosocial approach to care allows delivery of patient care in all life aspects including medical, psychological, and social. The biological aspect includes pharmaceutical care involving pharmacists and GP; psychological care involves psychologists and therapists who offer mental health support, and social workers and occupational therapists to improve social support and social processes.
Korsakoff’s syndrome is defined as a neuropsychiatric disorder damaging the various brain area to cause cognitive impairment and amnesia (Covell and Siddiqui, 2022). It has multiple etiologies but the most common, include chronic alcohol abuse leading to thiamine deficiency. Thiamine or vitamin B1 deficiency harms the brain and leads to confusion and other psychological issues. Mr Higgins had a history of excessive alcohol abuse, and his diagnosis can be attributed to this. Sharp et al. (2016) identified the signs and symptoms of Korsakoff’s syndrome, including altered mental status, such as disorientation, amnesia, and confabulations, which occurs in 82% of patients. Other symptoms include ataxia referred to as wide-based gait, and oculomotor nerve palsy, which interferes with the patient’s coordination, movement, and balance. Mr Higgins reported poor body balance and coordination while walking. Also, the disorder leads to retrograde amnesia, causing executive deficits in planning, judgment, and problem-solving abilities (Oudmanet al. 2015).
Moreover, the condition also leads to oculomotor abnormalities, mild memory deterioration, and dietary deficiency. Mr Higgins was not eating much and was severely losing weight, highlighting his cognitive impairment. To assess Mr Higgins’s care needs, a need assessment model was chosen to evaluate the care needs. The health need assessment of patients with severe psychological illnesses must aim to promote patients’ recovery rather than meeting their care needs (Werner, 2012). Psychological diseases not only cause medical issues, such as poor coordination and physical symptoms but also lead to psychotic conditions and psychological distress. It is crucial to identify and address these needs to eliminate the risk of severity and illness deterioration. Hence, the need assessment of an elderly patient with mental health issues must seek to improve the well-being of patients to avoid the risk of illnesses and make them a practical part of the community (Champion et al. 2017). For a comprehensive need assessment of Mr Higgins, Maslow’s Hierarchy of Needs was chosen. Maslow’s (1970) hierarchy of needs is the most popular and practicalsystem to enabling health need assessment. The approach is also practical as it not only recognises the care need but the motivation or driving force behind the need. The approach divides human needs into five core categories, including physiological, safety and security, love, self-esteem, and self-actualisation needs (Davison et al. 2021). These needs include food, water, shelter, healthcare, dignity, and social support (De Jong et al. 2017). Hence, it covers the biopsychosocial needs of patients by defining the patient’s health conditions in all life elements for delivering comprehensive care. The need assessment of Mr Higgins based on Maslow’s hierarchy of needs provides are.
1. Physiological needs
The physiological needs include nutrition, hydration, toileting, breathing, circulation, sleep, shelter, and sex needs. Mr Higgins was seen as severely malnourished and was losing weight. His difficulty in coordination and walking is limiting his ability to do physical exercise, which can lead to other health issues, such as the risk of cardiovascular diseases. Also, his case study showed that he was struggling with personal hygiene, showing his occupational inabilities and calling for occupational therapy.
2. Safety and security needs
The safety needs of patients include injury prevention and protection from the risk of viruses and infections. Also, older people are at increased risk of falls and require support in walking, sleeping, and other fall precautions. Mr Higgins has gait issues and poor body balance due to his Korsakoff syndrome and was vulnerable to falls. Thus, he needed support and care from a physiotherapist who would suggest him proper ways that can help him walk.
3. Love and belongingness needs
Love and belongingness need to include fostering practical relationships to prevent risk factors associated with isolation. Mr Higgins was divorced, but his ex-wife often visited him, and they both shared a friendly bond. However, lately, his ex-wife reported increased cases of aggression and frustration in him and incident of going violent toward his ex-wife and other people. It hampered his social relationships, making him vulnerable to isolation. Hence, he needed a psychologist or therapist who could meet his relationship needs and help him control his aggression.
4. Self-esteem needs
The self-esteem needs of a patient include personal achievements, confidence, and self-belief that can improve their self-worth. However, Mr Higgins was a journalist for a long time but now lived alone in his apartment and had health issues. His diagnosis and manifestations affected his health and social bonds, decreasing his self-esteem. Hence, his care needs also included practical education to make him realise his care needs and teach him self-management skills.
Goal setting
After assessing the patient’s needs, the next step is devising goals to improve their care. Patient-centred goal setting is one of the most practical interventions for rehabilitation (Smit et al. 2018). Goal setting for Mr Higgins involved active participation in the care process to deliver individualised care for him. However, patients with mental health issues and poor cognitive skills require the involvement of their families in care planning and goal setting. Patients having mental health issues need support from their families for performing their daily tasks, such as feeding, washing, cleaning, and medicine administration. Hence, families tend to ignore such patients and consider their burden and do not want to care for them. However, Mr Higgins had no family or other social groups that could help him in devising goals. Hence, as his social worker, I advocated on his behalf and collaborated with his ex-wife to design his care goals.
I conducted several sessions with Mr Higgins and his ex-wife, and with both to find his care preferences and needs. His care goals included:
- Care and support in movement and walking
- Improvement in cognitive functioning and thiamine levels
- Involvement in a social group, such as a political group to decrease isolation
- Educating the patient on self-management of his condition
- Occupational therapy to improve his hygiene and eating habits
Question 2
Adjustments to the care plan
Mr Higgins was under community care, before where he was receiving care for his alcohol addiction. He was on detoxification for his alcohol, but his care plan did not include consideration for his new diagnosis. After Korsakoff’s syndrome diagnosis, his care was shifted to the community mental health team where I worked as his social worker. My role within the care process for Mr Higgins was to devise a multidisciplinary team (MDT) to offer multilevel care for elderly patients and cater to their diverse needs.
Moreover, I needed to ensure that the care delivery was customised to meet the individual needs of both patients (Wintemute, 2021). The medium-term adjustments for Mr Higgins include coordinating different healthcare workers to improve the patient’s care. The long-term adjustments include arranging a community residence for him, which can ensure financial and social support and delivery of practical healthcare services for him. Customised or person-centred care is the core of healthcare practice as it allows one to consider the unique needs of the patients. It also involves offering therapeutic and counselling services for the patients to help them reach the healthcare providers. Hence, interprofessional team and person-centred care would allow me to cater to complex patients’ needs (Appendix A) and offer them efficient, safe, and practical MDT care using a biopsychosocial approach. Hence, the MDT will include professionals who will cater the biological, psychological, and social health needs of patients. A multidisciplinary Team (MDT) is a popular healthcare approach that enables the practical collaboration and coordination of healthcare workers and allied care professionals to improve the health outcomes of a single patient (SCIE, 2018). The significance of MDT for elderly patients is supported by most evidence showing the need for a care coordinator who can regulate the activities of care workers to increase patients’ autonomy and empowerment. My role within the MDT of Mr Higgins was coordinating the activities of various healthcare professionals based on my responsibilities listed in the code of practice. These responsibilities are included in Corus’ Domains and Proficiencies for social workers. The Health and Social Professional Act (HSCP Act, 2005) instructs registration boards to keep health and social care professionals. The board’s purpose is to safeguard the public by adopting ambitious standards of professional procedures and education, competence building, and training among the professionals (HSCP Act, 2005). The standard of proficiency includes professional accountability and autonomy, communication, collaboration and teamwork, safety and quality, professional development, and professional skills and knowledge. Hence, using my skills and expertise, I suggested a multidisciplinary team (MDT) for Mr Higgins, where I advocated his rights and first earned a financial grant for him from local government old-age benefit programs. Based on his recommendations from the general practitioner (GP), the budget included healthcare funds for his medical care and psychiatric care. The care Quality Commission (CQC, 2022) suggests that if the care for vulnerable adults is not coordinated practically, it can increase health risks for patients. Hence, before arranging Mr Higgins’s meeting with his care professionals, I sought to build rapport with him.
The most vital aspect of person-centred care and MDT care is improved communication skills and practical rapport building. The core of patient care is anpractical therapeutic relationship between patients and care providers. Practical communication allows for the identification of the patient’s needs and skill gaps in practitioners’ care delivery, which can reduce the patient’s outcomes. Mr Higgins had severe behavioural issues and would lash out at anyone trying to engage with him. Lopes, Afonso, and Ribeiro (2016) suggest making slight adjustments in the communication process while communicating with patients having mental health issues. Hence, in the first few sessions, I used small sentences, a warm tone, and a smiling face to introduce myself and my purpose of engaging with him. To prevent anger outbursts and any adverse response from him, I refrained from asking for details from him and let him develop the conversation and inform his issues. After building anpractical rapport with him, I only let his therapist talk to him and deliver the care. The initial plan was to send all care workers simultaneously, but I modified it based on Mr Higgins’s condition. For the first month, he only interacted with me and the therapist who helped him manage his anger. The therapist recommended social support for him as his anger issues were not only attributed to his withdrawal symptoms but also his isolation and lack of social support. NHS (2022) also recommends social support for the elderly as it can help improve their mental health and reduce vulnerability to psychological issues, such as depression and stress.
The initial care plan only included psychological interventions for Mr Higgins along with diet supplements and hence pharmacist was not included in the care plan. The dietician suggested hydration and vitamin B1 supplements to improve his care. However, the slight improvement in his condition led to the inclusion of a pharmacist who recommended thiamine replacement therapy for him. The following evidence from Sharp et al. (2016), 1000 mg of thiamine, three times a day was suggested for him for three days initially. The pharmacist administered the dosage intravenously rather than orally as he was reluctant to take medicine. Also, magnesium replacement therapy was included in his care plan to correct his fluid balance in the body. As he was severely undernourished and was not taking his meals properly, he was also given glucose replacement before thiamine therapy as thiamine is inpractical if the body lacks glucose (Covell and Siddique, 2022). Hence, his treatment included improving his hypoglycemia as prolonged hypoglycemia can increase the risk of Wernicke encephalopathy. After electrolyte replacement and vitamin B1 therapy, evidence recommends moving to memory rehabilitation for patients with Korsakoff syndrome. The therapist firstly focused on improving his procedural memory as it staysintact in the Korsakoff syndrome. Declarative memory is most affected in the disorder where the patient losses track of time, date, and people around them. It requires long-lasting care for supporting declarative memory; however, procedural memory can be improved with personalised care. Oudmanet al. (2015) state that patients can gain autonomy by learning procedures, and hence occupational therapist was included in MDT.
An occupational therapist was included in the team to offer technical aid by working in close collaboration with psychologists and physiotherapists (Soelberget al. 2019). The occupational therapist improved her daily routine performance, such as washing, eating, cooking, and maintaining personal hygiene. The physiotherapist and occupational therapist ensure his behavioural modifications ensuring his health promotion, practical rehabilitation, symptom management, and relapse prevention. The local agencies were also involved in the care that offered his financial grants and ensure practical intra-professional collaboration.
Mental health disorders impair complete life functioning, causing a severe deterioration in social and occupational functioning, and decreasing patients’ ability in performing life functioning. Mr Higgins was having issues in coordinating and balancing his body and thus physiotherapist suggested various exercise for him. The first exercise included a single limb stance with begins with a simple balance exercise for the elderly. The physiotherapist helped Mr Higgins to conduct this exercise by standing behind the solid chair holding its back and lifting the foot while shifting the weight on one foot. It allowed us to measure the foot’s ability to hold weight and improve balance and gait. Another exercise was a back leg raise, which includes strength training for the elderly, improving the strength in the lower back and bottom. These exercises allowed them to improve his posture and gait and decrease the risk of falling.
As his social worker, I planned his long-term care goals, which included changing his residence and providing him with a community apartment with adjustments to avoid the risk of falling. His room was on the ground floor and his bed included railings. The physiotherapist also includes crutches for him while walking to avoid falling and improve his balance. A community healthcare assistant was allocated to him as his ex-wife stated that she cannot care for him. Moreover, weekly community support group membership allowed them to decrease his isolation and improve his behavioural symptoms.
Question 3
3.0 Reflection
Reflection is the process of rethinking an incident for reaching a meaningful interpretation of the experience (Daryazadehet al. 2020). It allows to improve the awareness of an individual regarding the process and enhancing the future outcomes for students and practitioners. The present report was practical in guiding my learning regarding person-centred care and collaborative practice. The present reflection will be guided by Gibbs’s reflective model consisting of six stages, including description, feelings, evaluation, analysis, conclusions, and action plan. It is one of the most used frameworks in nursing that offer a structural model for nurses to perform reflection (Ahmed, 2019). It provides guiding questions for nurses to construct their reflection, but it does not include the perspective of other people, which decreases its practicality (Hopkinson, 2020).
3.1 Description
In the present case study, Mr Higgins had cognitive issues and was reluctant to collaborate with healthcare practitioners. The most critical issue in his care was building rapport with him and I realised that I lack practical communication skills to deliver individualised care for patients. Practical communication skills include developing rapport and understanding with patients, a proper language with no complex sentences, offering personal space, focusing on non-verbal communication, maintaining silence and eye contact, and actively listening to the patient.
3.2 Feelings
I felt bad for not having adequate communication skills to meet the health needs of patients. However, I was encouraged to improve my skills to improve rapport-building and communication skills for future practice.
3.3 Evaluation
I evaluate events as a learning experience as it develops my knowledge as a future social worker. Moreover, it facilitated me recognising a practice gap that is crucial to address. Communication skills are crucial for all healthcare and allied care practitioners, including social workers (Chichirez and Purcărea, 2018). Hence, I needed to improve my communication skills, including active listening and non-verbal communication.
3.4 Analysis
The most vital part of geriatric care is developing trust in them to help them open and share their issues. Also, the assessment report highlighted the need to include family members in the care of patients with mental health conditions. Kwame et al. (2021) stated that communication skills are the heart of person-centred care and professionals must improve them to enhance the care process. Moreover, Mr Higgins needed psychoeducation and as a care coordinator, I had a role in his care management and education. Thus, I needed to enhance my communication skills to become anpractical social work practitioner in the future.
3.4 Conclusion
From the experience, I concluded that rapport-building and practical communication are the heart of social work practice. Hence, developing these skills is paramount for my professional growth and development.
3.5 Action plan
To improve my communication skills, I undertook a training course for learning the art of active listening and non-verbal communication. The course also included practical sessions where we needed to interact with patients under the supervision of seniors for history intake and rapport building. The training was practical in improving my verbal and non-verbal skills and guiding my practice as a competent social worker in the future practice.
Reference
Chichirez, C. M.,and Purcărea, V. L., (2018). Interpersonal communication in healthcare. J Med Life,11(2), 119-122.
Coru, (2022). Social Care Workers Registration Board Standards of Proficiency for Social Care Workers.[online] Available at https://coru.ie/files-education/scwrb-standards-of-proficiency-for-social-care-workers.pdf
Covell, T., and Siddiqui, W.,(2022). Korsakoff Syndrome. StatPearls Publishing, [online] available at https://www.ncbi.nlm.nih.gov/books/NBK539854/
Gibbs, G., (1988). Learning by Doing: A guide to teaching and learning methods. Further Education Unit. Oxford Polytechnic: Oxford.
Oudman, E., Nijboer, T. C., Postma, A., Wijnia, J. W., Van der Stigchel, S.,(2015). Procedural Learning and Memory Rehabilitation in Korsakoff’s Syndrome – a Review of the Literature. Neuropsychol Rev,25(2), pp. 134-48.
Kwame, A., Petrucka, P.M. (2021). A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs, 20, 158.
NHS, (2022). Information sharing in Multidisciplinary Teams (MDTs).[online] Available at https://www.nhsx.nhs.uk/information-governance/guidance/information-governance-guidance-support-multidisciplinary-teams-mdts/
SCIE, (2022). Delivering integrated care: the role of the multidisciplinary team.[online] Available at https://www.scie.org.uk/integrated-care/workforce/role-multidisciplinary-team#:~:text=MDTs%20will%20provide%20a%20shared,to%20individuals%20and%20their%20families.
Sharp, C. S., Wilson, M. P., Nordstrom, K., (2016). Psychiatric Emergencies for Clinicians: Emergency Department Management of Wernicke-Korsakoff Syndrome. J Emerg Med, 51(4), pp. 401-404.
Smit, E. B.,Bouwstra, H., van der Wouden, J. C.,Wattel, L. M.,Hertogh, C. M. P. M., (2019). Patient-centred goal setting using functional outcome measures in geriatric rehabilitation: is it feasible? EurGeriatr Med,9(1), 71-76.