The present case study report will discuss the person-centred biopsychosocial assessment of the patient. It will highlight the one core care need of the patient and will use evidence-based tools to conduct her comprehensive biopsychosocial assessment. Moreover, it will discuss the role of registered nurse in the care process by forming therapeutic goals for patient using SMART tool. It will also point out the challenges in delivering evidence-based care including patient discharge, and communication within the organisation.
2.0 Case study
Following Nursing and Midwifery (NMC, 2019) code of confidentiality, the case study will use pseudonym Sarah for patient and Mike for her partner. Sarah, 30 years old mother of twins was recently admitted to Accident and Emergency (AED) department with extensive injuries on her wrist, arm, and thighs. Her assessment showed that she has history of self-harm and require effective wound management. During the clinical assessment, the nurse observed that Sarah was non-communicative and subdued and attributed her condition to excessive alcohol intake as shown by her blood sample. Her medical history showed that she was suffering from long periods of depression and was overdosing Sertraline, an antidepressant (NHS, 2022). Her medical history also showed bulimia and allergy to penicillin. Her BMI of 18 shows that she is on borderline of being underweight (NHS, 2022). She is physically active and sometimes overwork on her 150 minutes per week exercise and take minimum 4 units of alcohol, which is not alcoholic (NHS, 2022), and does not smoke. On admission to ward, her pain is settled but she is agitated and refuses to drink or eat anything as she feels anxious and depressed with her life. She also shows the signs of dehydration, which can be attributed to her depression, which is leading to self-harm, dehydration, and alcoholism. Thus, the core health need of Sarah identified in present case study is her depression.
3.0 Discussion
After identifying the core health need of Sarah, the ward nurse will conduct her assessment using evidence-based tool and will devise care plan for her. Moreover, it will highlight the potential challenges in the process that can limit the effectiveness of care process, and ways to mitigate these barriers.
Question 1
First, please identify and then discuss the key components or features of a person-centred bio-psychosocial assessment– you should do this in relation to the patient in the scenario. Secondly, expand upon and discuss how these key components or features relate specifically to one of the identified problems you have selected from the list above.
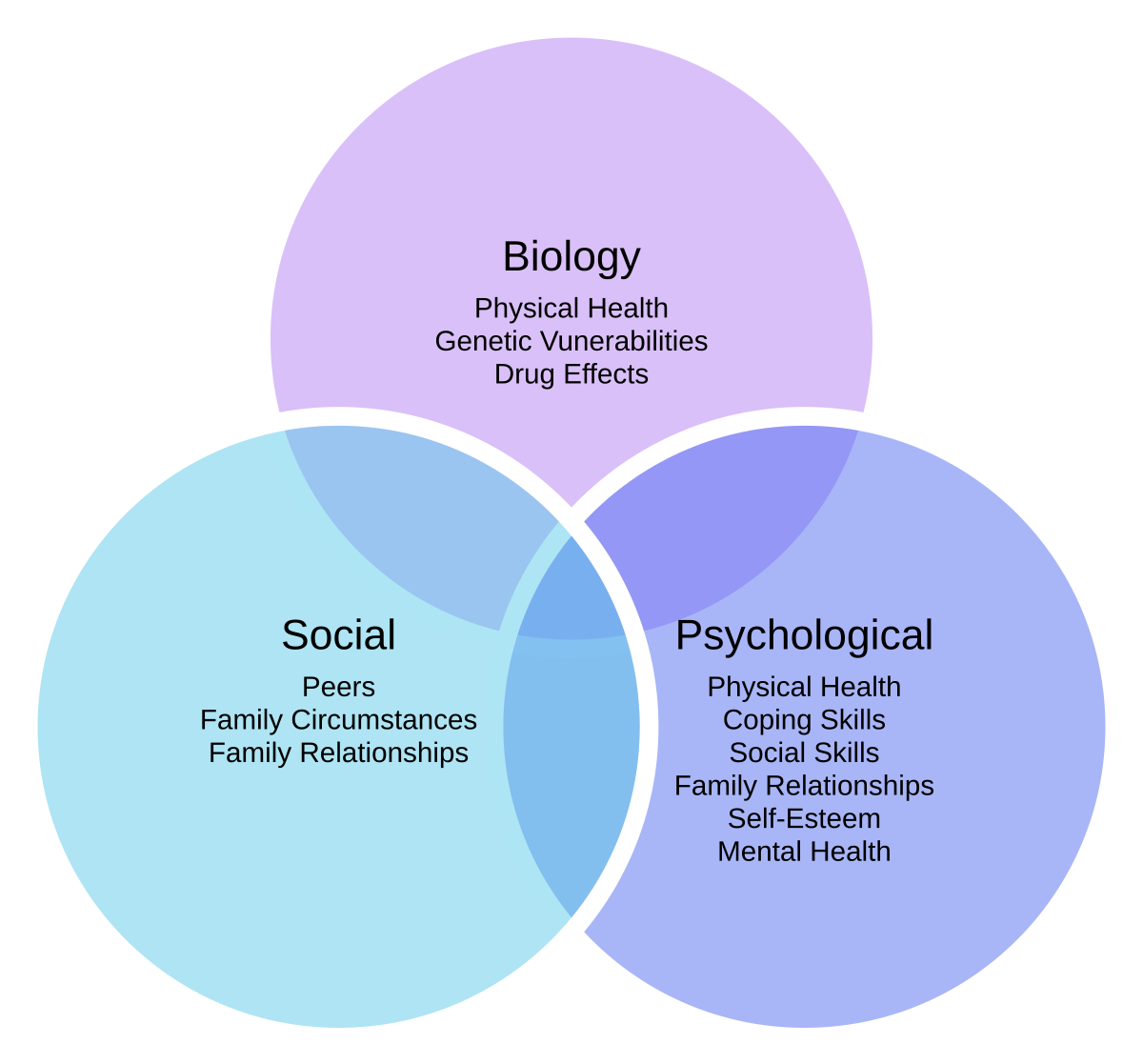
Engel (1977) developed the biopsychosocial model for caring for patient by assuming that the illness of the patient is attributable to blend of biological, psychological, and social factors noted in system hierarchy. The approach centres around patient, making them the core stakeholder and contributor to care process. Borrell-Carrio et al., (2018) provided the principles of biopsychosocial care of the patient that included calibrating the physician with patients’ needs. It refers to clinician ability to adjust with the patients’ needs to facilitate in rapport building. The other principles include creating trust, curiosity, recognition of biases, using intuitions, educating the emotions, and communicating the clinical evidence. The principles are important for person-centred care of the patient that values the patients’ needs, preferences, and values of the patient (Pinho et al., 2021). One central focus on person-centred care is shared decision-making that involves the patients and care professionals, information sharing between both parties, informed and collaborative decisions of patients’ treatment, and consensus for execution of care plan (Aljaffary et al., 2022). Therefore, the core component of person-centred assessment and management of patient is shared decision-making that focus on patients’ experiences.
NICE (2009) guidelines concerning the assessment and management of depression in adults inform that evaluation of patients with depression must be comprehensive not merely symptom count. Additionally, it should account the extent of functional impairment and disability linked to depression and duration of episode. Durham University (2022) has also pointed out the principles of patient assessment that provide that the assessment tools must be valid, reliable, transparent, explicit, efficient, and equitable. Hence, the key component of ideal assessment tool for patients include: time-consuming tools such as self-reported measures, which can collect information like interviews and encourage logical inferences. Therefore, present report will use Formal Psychological Assessment (FPA), a complex tool used for collecting, analysing, and processing patients’ information (Spoto et al., 2013).
Formal Psychological Assessment (FPA) seeks to enhance the procedures by offering formal framework for building assessment tools. Serra et al., (2015) used the FPA for patients with depression posing that it has capacity to maximise the benefits of both self-reported measures and semi-structured interviews by overcoming the limitations of individual tools used for traditional assessment.
- Beck Depression Inventory (BDI)
Aaron Beck with his colleagues (1961) created BDI for assessing the patients with depression. The current version of BDI consist of 21 questions with score for each question ranging from 0-3. The higher the score, the more severe the depression is in patients. The tool is extensively used in the clinical setting by the psychiatric nurses as it is valid and culturally appropriate (Seppanen et al., 2022). It can predict the depressive symptoms and their severity in patients and offer clinically significant findings. However, the high item difficulty, controversial factorial validity, and scores instability impact its validity (Wang and Gorenstein, 2021). Moreover, it has poor discrimination validity against anxiety; thus, other tools are used along with it to confirm diagnosis.
- Zung Self-Rating Depression Scale (SDS)
Zung et al., (2019) developed Zung Self-Rating Depression Scale for assessing symptom severity in patients with depression. It consists of 20 items that measure the psychological, affective, somatic symptoms of depression. As the tool is quick and simple, nurses extensively use it in clinical settings to assess the patients with depression (APA, 2022). However, self-reported measures are bound to social desirability bias limiting their effectiveness.
- Beck Hopelessness Scale
The Beck Hopelessness Scale is self-reported measure used for adults to assess the negative expectations about the future (Beck et al., 1974). The 20 items scale include dichotomous responses to questions and takes around 5 minutes to complete. David Klonsky et al., (2012) has established the predictive validity of the scale and is good measure of suicidal ideation, hopelessness, and psychotic symptoms in patients. It is equally feasible to use in inpatient and outpatient in medical and psychiatric populations (Korkmaz et al., 2019). Moreover, it can predict the social functioning and general health status in psychiatric sample.
- Hamilton Rating Scale for Depression
The Hamilton Rating Scale for Depression or HAM-D is evidence-based measure for depression in individuals and allow comparing the symptoms before, during, and after the treatment (Hamilton, 1960). The scale is clinician-rated measure and healthcare professionals administer the 21-items, but only 17 items are scored on 3-5 points measures. It covers the limitations of self-rated measure reducing the social desirability bias and offer more informed judgment of patient’s condition. However, Carrozzino et al., (2020) noted the limitations of the scale such as its inability to cover the diagnostic criteria of depression in DSM diagnostic criteria. The limited coverage of the depressive symptom decreases its utility as a diagnostic measure.
These scales were used to assess Sarah as it covered her self-harm, which potentially indicated suicidal ideations. The assessment allowed to devise evidence-based car plan for her to improve her depressive symptoms.
Question 2
Discuss the role of the registered nurse when planning, implementing, and evaluating evidenced based care for the patient in the scenario, relating this specifically to the one identified problem you selected in question 1. Please discuss how relevant evidenced based theory in relation to your chosen problem should be applied to clinical practice.
The treatment response of the major depressive disorder is usually assessed via traditional mental health professional and patient self-reported scales (McCue et al., 2021). These scales emphasise on the evident indications; however, these tools do not include the substantial changes regarding the specific condition of the patient. A contemporary tool which addresses the importance of response to management in an individualised manner is one that utilises the Goal Attainment Scale (GAS), formulated by Kiresuk and Sherman (1968). This assessment tool constitutes of semi-quantitative approach which incorporates patients’ personal preferences and what they hope to achieve from the treatment by evaluating the outcomes against SMART goals (specific, measurable, attainable, relevant, and time-bound (Krasny-Pacini et al., 2013), which allows for adequate inter-rater reliability. The outcomes were also evaluated via GAS complement traditional clinical scales which is useful to measure progress in treatment goals and/or outcomes. These outcomes are important and integral for patients to maintain holistic wellbeing which is otherwise challenging to accept (Gaasterland et al., 2016). Setting goals of the care can assist the patient in moving towards desired treatment outcomes in relation to appropriate behavioural modifications and can increase engagement with the healthcare professionals (Cairns et al., 2019). Goal setting and defining treatment success as goal achievement are integral to cognitive behavioral therapy (CBT) and to the application of the GAS adapted for depression (GAS-D) approach for patients with depression. Both approaches involve identifying a behavior associated with the symptoms of depression and setting goals representing a desirable behavior change. As part of the CBT process, the set goals are regularly reexamined, challenges to the care implementation are addressed, and drives to achieve goals are reinforced (Fenn and Byrne, 2013). On the other hand, goal setting using the GAS-D approach occurs before initiating therapy, and progress against these goals is assessed without active follow-up or reinforcement, offering a novel method of investigating the efficacy of pharmacologic therapies. The goals for Sarah involved improving her psychiatric care, hydration, and decreasing instances of self-harm using CBT. Moreover, it will involve a person-centred care and shared decision-making approach enforced by the certain queries which will be inquired from the patient (Sarah) to ask for her explanation of the causes behind her condition, and what she considers the best way to manage her problem. Therefore, key early questions in the clinical interview include: “What do you think is going on?” and “Based on that, what do you think is the best way forward?”. The Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 cultural formulation interview can be used as well to ensure a complete understanding of the condition (McCue et al., 2021). So making the process individualised for her helped in enhancing her wellbeing and decreasing chances of relapse of symptoms.
Psychiatry presently aims to personalized medicine, where the care plan is formulated on the holistic needs of the patients including genetic, environmental, and sociocultural (McCue et al., 2021). The dosage of her Sertraline was increased to help her with severe depression. Anxious depression is associated with increased intensity, elevated suicidal ideation, and overall worst outcomes in contrast to depressive symptoms which are not linked with anxiety (Gaasterland et al., 2016). Thus, depressive patient comorbid with anxiety require vigorous care planning and treatment. Generally, there is inadequate evidence demonstrating that one category of ant—depressions are more effective than ones for anxious depression (Krasny-Pacini et al., 2016). Nevertheless, a systematic review of 6 clinical trials of agomelatine reported a significant impact in earlier days (two-four weeks) for anxiety symptoms in depressive patients receiving agomelatine in contrast to participants receiving placebo, serotonin norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors (Cairns et al., 2019). The variations in the effect of agomelatine on the Hamilton Depression Rating Scale subscores in comparsion to placebo was significantly high in anxiety patients, thus concluding that agomelatine have significantly higher effects on anxiety and depressive symptoms as compared to other relevant antidepression agents (Cairns et al., 2019).
Registered nurses (RN) have outmost important role in the care planning and implementation process. Thus, registered nurses are well-placed for the identification, assessment, and intervention (in accordance with the care need) against depressive symptoms among elderly people (Winkley, 2013). They are deemed essential and vital in reducing the adverse consequences of depressive symptoms via the use of relatable and time-effective evidence-based intervention. However, RNs seldom recognises the depressive symptoms in elderly people (Waterworth et al., 2015). Inadequate knowledge about depression and its symptoms and lack of confidence can be possible factors in RNs inability to identify and discuss depression with service users (Barker et al., 2014). Another reason can be RN’s belief that they are not responsible to identify depression in patients and it’s beyond the scope of their practice (Waterworth et al., 2015). Regardless of the clinical setting, registered nurses demonstrated that it was challenging to accurately identify depression in elderly people, yet a systematic review indicated that still they were as successful as GPs (Mitchell and Kakkadasam, 2011). There is a significance of identifying depression or depressive symptoms in elderly people and implement an efficient approach to provide care to the patients. Thus, registered nurses in primary care setting have a particularly significant role to play in the offering care to the elderly people experiencing depressive symptoms and/or depression.
Question 3
Identify and then discuss the challenges faced when providing (implementing) effective evidenced based care for the patient in the scenario, including discharge planning, referral to other services and transition to the primary care team.
Evidence-based care is regarded as most effective care for patients as it uses the best available research to deliver appropriate care for patients. However, integrating the evidence into clinical practice is challenging for healthcare professionals (McArthur et al., 2021). The studies guiding the nursing utilisation and adherence to evidence found that large percentage of evidence are not properly implemented (Micken et al., 2011). Surprisingly, the senior nursing professional have negative attitude towards application of evidence into care. However, with NHS and NICE issuing guidelines on importance and need of implementation of evidence-based care, they have adopted the practice in care process (Fakirayya and Pushpa, 2022). Another significant barrier in implementation of evidence-based care is knowledge gap existing between the information within the guidelines, disinterest of nurses, and fatigue attached with change process decrease the motivation and psychological capacity of the nurses to adopt the practice in their routine care (McArthur et al., 2021). The allied and nursing care workers with limited education, having low wages and compensation, restricted autonomy, decreased job satisfaction, and work-related burnout avoid using evidence-based measures (Caspar et al., 2016). One of the widely reported organisational barriers in application of evidence-based care is lack of human resources such as nurses, non-availability and access to internet at work, inaccessibility to evidence rich libraries and journals, and increased workload contribute to decrease in care quality. Varaei et al., (2013) stated that heavy workloads and nursing shortage are among strong constraints for nurses and decrease nurses’ willingness to participate in care process. another research determining the association between nurses personal and professional factors and evidence-based care stated that 32% nurses do not have access to evidence rich library and 42% do not have internet facilities at workplace (Mashiach Eizenberg, 2011). Additionally, the availability of the human resource is biggest facilitator in evidence-based care along with organisational support. Therefore, effective organisational strategies can increase the awareness and motivation of the nurses to follow the practice (Khammarnia et al., 2015). Moreover, the issues related to appraisal and understanding of the evidence are related to organisational context and effective organisational policies can mitigate them. Thus, changing the appraisal system within the organisation can support the use of quality evidence in patient care (Nikpeyma et al., 2014). These barriers were effectively catered in Sarah’s care where the experienced professionals with required knowledge were included in the care process of patient.
However, nurses encountered barriers in her discharge planning where lack of communication impacted the process. Okoniewska et al., (2015) identified various obstacles in discharge process including such as communication, issues related role clarity, lack of human and organisational resources, structure and function of the medical team, and need for leadership. As identified in the case study, Sarah was reluctant to cooperate with the care professionals as she was extensively anxious and worried about her life. It was extremely difficult for the nurses to educate her on her care plan and discharge her to her home. Therefore, psychiatrist was involved in the process who through effective rapport building facilitated her to understand the importance of life and why she should live for her daughters. Though her children were very little to become part of her comprehensive care planning, but psychiatrist mentioned them many times to convince Sarah to skip self-harming behaviour and improve her life. She was discharged into primary care process as her self-harming behaviour was not under control and required continuous care. Primary care workers are crucial in identifying and managing depression. Around 60% of mental care delivery take place in the primary care units (Park and Zarate, 2019). Thus, her discharge into primary care allowed to continue her care and involve multiple professionals in her care to deal with her dehydration and wound management. The tissue viability nurse, psychiatrist, and community nurse visited her every week to ensure that she was following the care plan.
- Conclusion
The present essay discussed the case study of Sarah who was undergoing depression with multiple needs including dehydration, pain, and wound management. In first step comprehensive assessment of her condition was performed to judge the severity of her symptoms. In second step, her care goals were devised using GAS-D approach and in last step barriers in her care were identified to improve her condition.
5.0 References
Aljaffary, A., Alsheddi, F., Alzahrani, R., Alamoudi, S., Aljuwair, M., Alrawiai, S., Aljabri, D., Althumairi, A., Hariri, B., & Alumran, A. 2022. Shared Decision-Making: A Cross-Sectional Study Assessing Patients Awareness and Preferences in Saudi Arabia. Patient preference and adherence, 16, pp. 1005–1015. https://doi.org/10.2147/PPA.S332638
Barker, S., Heaslip, V., Chelvanayagam, S. 2014. Addressing older people’s mental health need in the community setting. Br J Community Nurs, 19(5), pp. 234–8. https://doi.org/10.12968/bjcn.2014.19.5.234.
Beck, A.T., Weissman, A., Lester, D., and Trexler, L. 1974. The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology, 42(6), pp. 861-865. http://dx.doi.org/10.1037/h0037562
Beck, A.T., Ward, C.H., Mendelson, M., Mock, J., and Erbaugh, J. 1961. An inventory for measuring depression. Archives of General Psychiatry, 4(6), pp. 561-571. http://dx.doi.org/10.1001/archpsyc.1961.01710120031004
Borrell-Carrió, F., Suchman, A. L., and Epstein, R. M. 2004. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Annals of family medicine, 2(6), pp. 576–582. https://doi.org/10.1370/afm.245
Cairns, A. J., Kavanagh, D. J., Dark, F., McPhail, S. M. 2019. Goal setting improves retention in youth mental health: a cross-sectional analysis. Child Adolesc Psychiatry Ment Health, 13, pp. 31.
Carrozzino D. Patierno C. Fava G. Guidi J. 2020. The Hamilton Rating Scales for Depression: A Critical Review of Clinimetric Properties of Different Versions. Psychother Psychosom, 89, pp. 133–150.
Caspar, S., Ratner, P. A., Phinney, A., MacKinnon, K. 2016. The influence of organizational systems on information exchange in long-term care facilities. Qual Health Res, 26(7), pp. 951–65.
David Klonsky, E., Kotov, R., Bakst, S., Rabinowitz, J., Bromet, E. J. 2012. Hopelessness as a predictor of attempted suicide among first admission patients with psychosis: a 10-year cohort study. Suicide Life-Threat Behav, 42(1), pp. 1–10.
Durham University, 2022. Principles of Assessment. [online] Available at: https://www.dur.ac.uk/learningandteaching.handbook/6/principles/
Engel, G. L. 1977. The need for a new medical model: A challenge for biomedicine. Science, 196, pp. 129–36.
Fakirayya, K. Pushpa, K. 2022. Challenges for the practice of evidence-based medicine during COVID-19 pandemic (practice of evidence-based medicine in the new normal). Indian Journal of Anaesthesia, 66(4), pp. 290-293.
Gaasterland, C. M., Jansen-van der, Weide, M. C., Weinreich, S. S., van der Lee, J. H. 2016. A systematic review to investigate the measurement properties of goal attainment scaling, towards use in drug trials. BMC Med Res Methodol, 16, pp. 99.
Hamilton, M. 1960. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry, 23, pp. 56-61. http://dx.doi.org/10.1136/jnnp.23.1.56
Khammarnia, M., Haj Mohammadi, M., Amani, Z., Rezaeian, S., and Setoodehzadeh, F. 2015. Barriers to implementation of evidence based practice in zahedan teaching hospitals, Iran, 2014. Nursing research and practice, 2015, 357140. https://doi.org/10.1155/2015/357140
Korkmaz, H., Korkmaz, S., Çakar, M. 2019. Suicide risk in chronic heart failure patients and its association with depression, hopelessness and self esteem. J Clin Neurosci, 68, pp. 51–4.
Krasny-Pacini, A., Hiebel, J., Pauly, F., Godon, S., Chevignard, M. 2013. Goal attainment scaling in rehabilitation: a literature-based update. Ann Phys Rehabil Med, 56, pp. 212–30.
Mashiach Eizenberg M. 2011. Implementation of evidence-based nursing practice: nurses’ personal and professional factors? Journal of Advanced Nursing, 67(1), pp. 33–42.
McArthur, C., Bai, Y., Hewston, P. 2021. Barriers and facilitators to implementing evidence-based guidelines in long-term care: a qualitative evidence synthesis. Implementation Sci, 16, pp. 70.
Mickan, S., Burls, A., Glasziou, P. 2011. Patterns of “leakage” in the utilisation of clinical guidelines: a systematic review. Postgrad Med J, 87(1032), pp. 670–9.
Mitchell, A. J., Kakkadasam, V. 2011. Ability of nurses to identify depression in primary care, secondary care and nursing homes—a meta-analysis of routine clinical accuracy. Int J Nurs Stud, 48(3), pp. 359–68. https://doi.org/10.1016/j.ijnurstu.2010.05.012.
NICE, 2009. Depression in adults: recognition and management. [online] Available at: https://www.nice.org.uk/guidance/cg90/chapter/key-priorities-for-implementation#principles-for-assessment
NHS, 2022. Sertraline. [online] Available at: https://www.nhs.uk/medicines/sertraline/
NHS, 2022. BMI healthy weight calculator. [online] Available at: https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
NHS, 2022. Alcohol misuse. [online] Available at: https://www.nhs.uk/conditions/alcohol-misuse/
Nikpeyma N., Abed-saeedi Z., Azargashb E., Alavi-majd H. 2014. Problems of clinical nurse performance appraisal system: a qualitative study. Asian Nursing Research, 8(1), pp. 15–22.
Park, L. T., & Zarate, C. A., Jr. 2019. Depression in the Primary Care Setting. The New England journal of medicine, 380(6), pp. 559–568. https://doi.org/10.1056/NEJMcp1712493
Okoniewska, B., Santana, M. J., Groshaus, H., Stajkovic, S., Cowles, J., Chakrovorty, D., and Ghali, W. A. 2015. Barriers to discharge in an acute care medical teaching unit: a qualitative analysis of health providers’ perceptions. Journal of multidisciplinary healthcare, 8, pp. 83–89. https://doi.org/10.2147/JMDH.S72633
Pinho, L. G., Lopes, M. J., Correia, T., Sampaio, F., Arco, H., Mendes, A., Marques, M., and Fonseca, C. 2021. Patient-Centered Care for Patients with Depression or Anxiety Disorder: An Integrative Review. Journal of personalized medicine, 11(8), pp. 776. https://doi.org/10.3390/jpm11080776
Seppanen, M., Lankila, T., Auvinen, J., Miettunen, J., Korpelainen, R., and Timonen, M. 2022. Cross-cultural comparison of depressive symptoms on the Beck Depression Inventory-II, across six population samples. BJPsych open, 8(2), pp. 46. https://doi.org/10.1192/bjo.2022.13
Serra, F., Spoto, A., Ghisi, M., and Vidotto, G. 2015. Formal psychological assessment in evaluating depression: a new methodology to build exhaustive and irredundant adaptive questionnaires. PloS one, 10(4), e0122131. https://doi.org/10.1371/journal.pone.0122131
Varaei S., Salsali M., Cheraghi M. A. 2013. Implementation of evidence-based nursing practice for diabetic patients: an Iranian experience. International Journal of Nursing Practice, 19(supplement 3), pp. 73–80.
Wang, Y. and Gorenstein, C. 2021. Chapter 16 – The Beck depression inventory: Uses and applications. In The Neuroscience of Depression.
Waterworth, S., Arroll, B., Raphael, D., Parsons, J., Gott, M. 2015. A qualitative study of nurses ‘clinical experience in recognizing low mood and depression in older patients with multiple long-term conditions. J Clin Nurs, 24(17–18), pp. 2562–70. https://doi.org/10.1111/jocn.12863.
Winkley, K. 2013. Depression and diabetes: what should nurses do? Nurs Times, 109(45), pp. 20–2.